Esomeprazol (PPI) vs. Fundoplicatio bei Reflux(GERD)
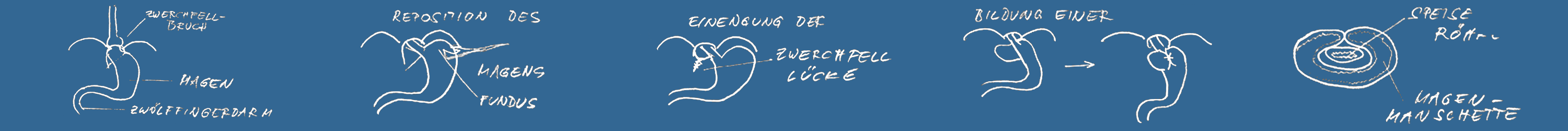
The three year results of a manufacturer sponsored randomized trial comparing laparoscopic fundoplication and esomeprazol (the Lotus study) were published in 2008 (Lundell 2008). Following fundoplication 90 % of patients were satisfactorily freed from reflux symptoms after three years, as well as 93% of the patients on esomeprazole therapy (NS). Significantly more patients suffered from heartburn and regurgitation in the medical group, indicating a more complete symptom control after surgery (p<0.001). Dysphagia – mostly mild – was reported by around only 15% of patients after surgery – fewer than preoperatively (18%), and by 4 % in the medical group. Flatulence was encountered in more patients in the fundoplication group. Quality of life scores showed greater improvement in the surgical than in the medical patients for all QOLRAD (quality of life in reflux and dyspepsia) dimensions and for the reflux dimensions of the GSRS (gastrointestinal symptom rating scale) questionnaire (p<0.001). Only 3% complications occurred after fundoplication during the hospital stay or the 30 postoperative days. There was no mortality after surgery, one patient succumbed to pneumonia in the medical arm. In 3.8% of the medical patients adverse events led to discontinuation of the study, as compared to 0.8% in the surgical group. The trial revealed that laparoscopic fundoplication is a safe and very effective treatment for gastrooesopageal reflux. The procedure is associated with a very low morbidity and no mortality if carried out in experienced high-volume institutions. Symptom control after three years is more complete following operation, and quality of life scores are better in the surgical group.
The treatment efficacy after longer time intervals is not yet known, and the results after more than five years will probably never turn up, since Astra-Zeneca, the manufacturer of esomeprazol, decided to discontinue the study in summer 2008. The reason for this move is not quite clear. An earlier study which compared open fundoplication with omeprazol revealed no significant results after five years, but a higher proportion of patients remaining symptom-free after seven years (L. Lundell 2007). In that trial treatment did not fail in 67% of the surgical (fundoplication) patients and in 47% of the medical group (p=0.002). Hovever, a significant difference had not shown up after shorter observation intervals, suggesting that PPI treatment lost it’s efficacy at a faster pace than fundoplication. Observational studies after laparoscopic fundoplication revealed that after a median follow-up of eight years only around 12 % symptomatic recurrences were observed (J. Hafez 2008). The criteria to define treatment failure were the same as in the Lotus study. The median interval between operation and recurrence was 30 months. The majority of recurrences (14 of 16 cases; 88%) were encountered within 36 months after surgery, and no recurrence had arisen later than 69 months postop. Should the recurrences behave similarly in the Lotus study, superior and longer-lastig reflux control should be expected in the fundoplication group. It is therefore deplorabe that the sponsor terminated the study before longer lasting observations had been carried out. Obviously there was no economical incentive to be expected in a trial showing the superiority of surgical treatment.
Esomeprazol (PPI) vs. fundoplication gastroesophageal reflux disease (GERD)
The three year results of a  manufacturer sponsored randomized trial comparing laparoscopic fundoplication and esomeprazol (the Lotus study) were published recently (Lundell 2008). Following fundoplication 90 % of patients were satisfactorily freed from reflux symptoms after three years, as well as 93%  of the patients on esomeprazole therapy (NS). Significantly more patients suffered from  heartburn and regurgitation in the medical group, indicating a more complete symptom control after surgery (p<0.001). Dysphagia – mostly mild –  was reported by around only 15% of patients after surgery – fewer than preoperatively (18%), and by 4 % in the medical group. Flatulence was encountered in more patients in the fundoplication group. Quality of life scores showed greater improvement in the surgical than in the medical patients for all QOLRAD (quality of life in reflux and dyspepsia) dimensions and for the reflux dimensions of the GSRS (gastrointestinal symptom rating scale) questionnaire (p<0.001). Only 3% complications occurred after fundoplication during the hospital stay or the 30 postoperative days. There was no mortality after surgery, one patient succumbed to pneumonia in the medical arm. In 3.8% of the medical patients adverse events led to discontinuation of the study, as compared to 0.8% in the surgical group. The trial revealed that laparoscopic fundoplication is a safe and very effective treatment for gastrooesopageal reflux. The procedure is associated with a very low morbidity and no mortality if carried out in experienced high-volume institutions. Symptom control  after three years is more complete following operation, and quality of life scores are better in the surgical group.
The treatment efficacy after longer time intervals is not yet known,  and the results after more than five years will probably never turn up, since Astra-Zeneca, the manufacturer of esomeprazol, decided to discontinue the study in summer 2008. The reason for this move is not quite clear. An earlier study which compared open fundoplication with omeprazol revealed no significant results after five years, but a higher proportion of patients remaining symptom-free after seven years  (L. Lundell 2007). In that trial  treatment  did not fail in  67% of the surgical (fundoplication) patients and in 47% of the medical group (p=0.002). Hovever, a significant difference had not shown up after shorter observation intervals, suggesting that PPI treatment lost it’s efficacy at a faster pace than fundoplication. Observational studies after laparoscopic fundoplication revealed that after a median follow-up of eight years  only around 12 % symptomatic recurrences were observed (J. Hafez 2008). The criteria to define treatment failure were the same as in the Lotus study.  The median interval between  operation and recurrence was 30 months. The majority of recurrences (14 of 16 cases; 88%) were encountered within 36 months after surgery, and no recurrence had arisen later than 69 months postop. Should the recurrences behave similarly in the Lotus study, superior and longer-lastig reflux control should be expected in the fundoplication group.   It is therefore deplorabe that the sponsor terminated the study before longer lasting observations had been carried out.